How AI is helping health programs in Africa move from faster delivery to individualized engagement and why this matters for closing the health engagement gap.
The Engagement Gap in Health Systems
Across Sub-Saharan Africa, health systems have made major strides in expanding infrastructure, from electronic health records, DHIS2 registries, CRMs, even mobile-based reporting. But these systems are mostly built to record, not to engage. They capture data but often fail to close the loop back to people.
Health communication tools, from mass media campaigns to SMS alerts to community health workers, push content out, but very little ties it together in real time. The result:
- Engagement gaps: health systems cannot answer who should get what message, when, or why.
- Referral gaps: people are not connected to the right service at the right time.
- Feedback gaps: frontline insights are slow to reach decision-makers.
Bridging these gaps is essential. Without a context-aware approach to orchestrate communication, systems remain fragmented, non-adaptive, and out of sync with frontline realities.
Why the Old Production Process Is Struggling
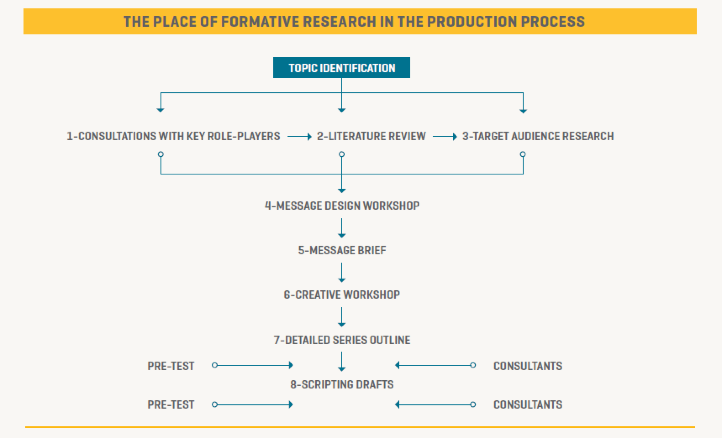
Traditional SBCC (Social and Behavior Change Communication) workflows depend heavily on linear research and campaign development cycles:
- Consult key role players
- Conduct literature reviews and audience research
- Design messages in workshops
- Pre-test and script drafts
This model, based on the formative audience research process works, but it is too slow and resource-heavy for fast-changing health environments. Campaigns are often outdated by the time they reach communities. In emergencies like pandemics or in dynamic health contexts like chronic disease management, this lag is costly.
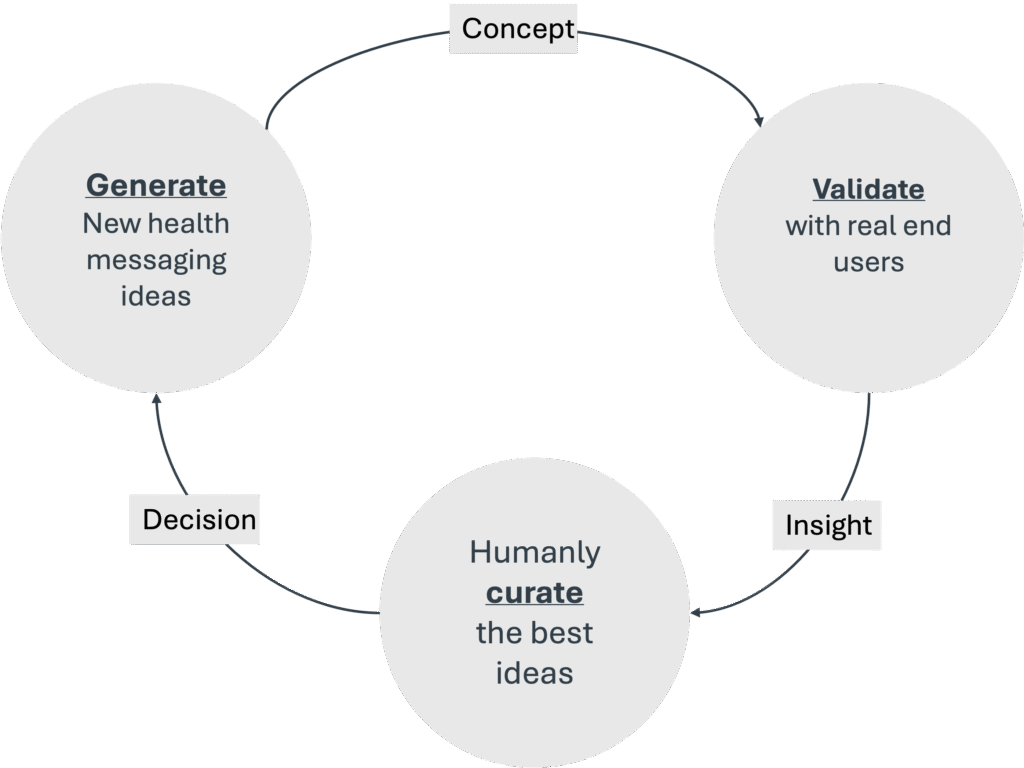
A New Cycle: Generate, then Validate, then Curate
We propose a shift away from rigid, one-off campaign design toward a continuous innovation cycle powered by AI. Instead of waiting months to finalize campaigns, health programs could:
- Generate new health messaging ideas at scale (e.g., personalized SMS prompts, chatbot conversations).
- Validate these messages quickly with real end-users in different contexts (via rapid prototyping and structured feedback loops).
- Curate the best-performing ideas, with human oversight ensuring cultural relevance, safety, and accuracy.
This cycle is not just theoretical – it points to a more agile future where health programs learn from every interaction and can adapt as conditions change.
The Three Waves of AI Adoption in Health Programming
Much like video technology evolved from basic editing to real-time personalized experiences, AI in health program delivery is moving through three waves:
- Wave 1 – Faster & Cheaper
- Use AI to automate repetitive work like health message drafting, translation, or campaign reporting.
- Example: Rapidly generating reminders for malaria treatment or vaccination.
- Wave 2 – Better Quality
- Move from generic content to behaviorally informed, context-aware messages.
- Example: Chatbots that adapt tone and framing for caregivers vs. adolescents vs. CHVs.
- Wave 3 – Individualized Real-Time Engagement
- Deliver health journeys that adapt in real time to each person’s needs.
- Example: A caregiver receives the exact malaria dosing reminder for their child, linked to clinic schedules, in the language they prefer.
This is the shift from “content push” to “decision support” for both people and health workers.
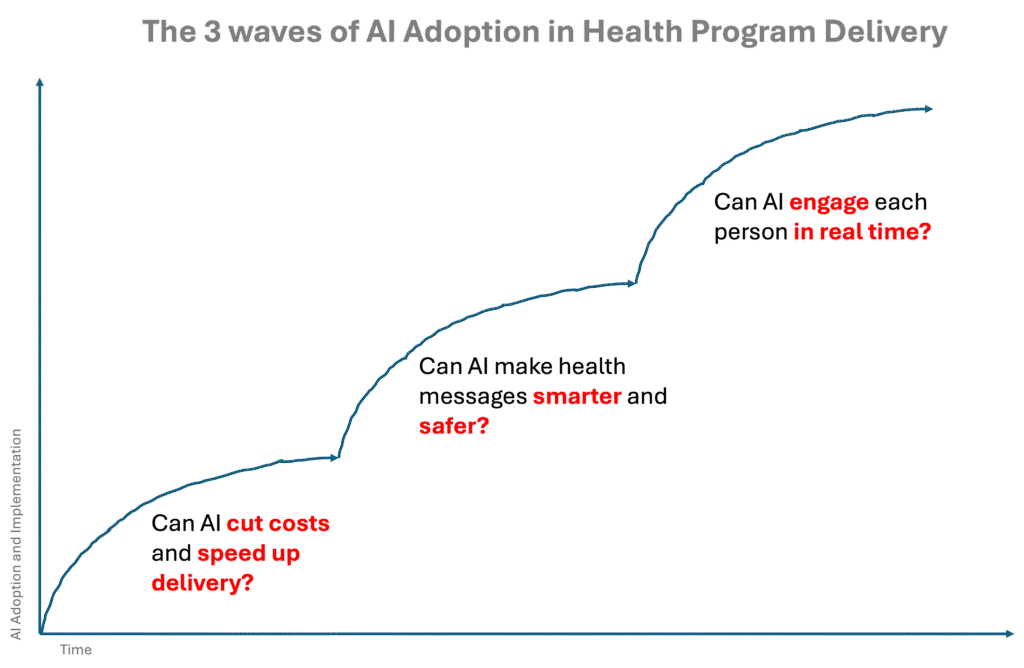
The three waves of AI adoption in health delivery, faster and cheaper, better quality, and individualized real-time engagement, may sound like a distant horizon. But in reality, the first ripples of these waves are already here. We see them in incremental capabilities that, once deployed, start compounding value across health systems.
Take three examples:
- Optimized, continuously improving insights: AI can already help extract signals from messy program data, generate tailored content, and support better decision-making. For health programs, this means lowering the cost of intervention design while improving satisfaction because messages and campaigns are grounded in real evidence, not guesswork.
- Real-time AI co-pilots: Copilots embedded in workflows from chatbot assistants for frontline workers to message generators for campaign teams are reducing risks by keeping advice consistent, contextual, and grounded in guidelines. These copilots improve satisfaction for both providers and users by making health interactions smoother and more trustworthy.
- Frontline-facing channels and chatbots: Purpose-built bots for priority populations can boost productivity while reducing cost. Think of bots that handle reminders, answer FAQs, or triage routine queries, freeing up scarce human resources for the tasks that matter most.
Each of these capabilities draws on the same underlying Generative AI strengths, insights extraction, user interaction, and content generation. But when layered together, they do more than solve individual problems. They start creating a multiplier effect: one improvement in messaging sharpens demand generation, which improves service uptake, which generates better data, which feeds back into smarter messaging.
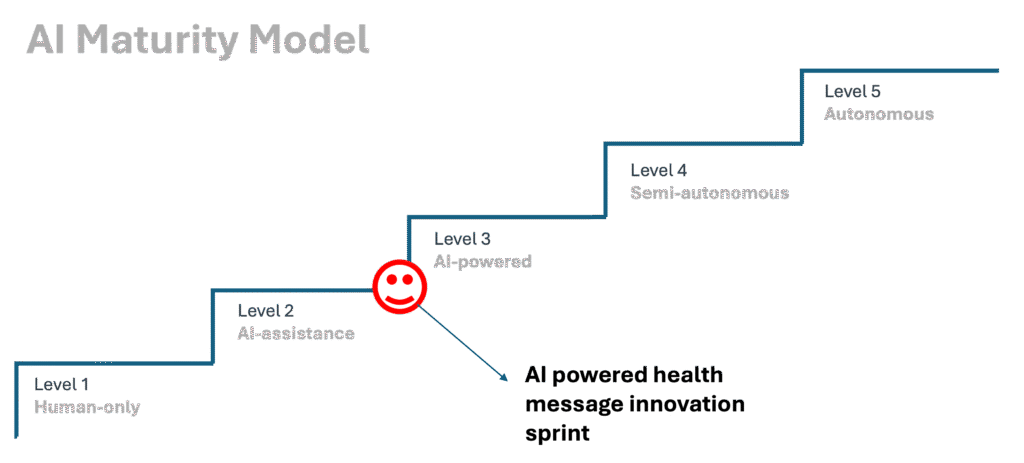
The AI Maturity Model: Crossing the Waves
To move across these waves, health systems need a clear maturity pathway:
- Level 1 – Human-Only: Campaigns designed and delivered without AI.
- Level 2 – AI Assistance: AI supports drafting, analysis, or translation, but humans lead.
- Level 3 – AI Powered: AI actively generates and adapts messaging, validated by humans.
- Level 4 – Semi-Autonomous: AI systems orchestrate engagement across channels, with human oversight.
- Level 5 – Autonomous: Fully adaptive systems that learn continuously from data and optimize messaging in real time.
For DPE and solution such as InfoAFYA™ & InfoAFYA+, this pathway is already in motion – with AI-powered message innovation sprints helping health programs test and scale new strategies faster. This is one of the core use cases for the LLM model we have recently developed. We will be publishing more about what we are learning from these sprints. We genuinely believe that the health sector is ready to quickly shift from level 1 to level 4, to varying degrees.
Closing the Gap: From Linear to Exponential Health Programs
The story of AI adoption in health program delivery isn’t just about new tools, it’s about a fundamental shift in operating behaviors. For too long, health systems have been bound by linear processes, resource-heavy scaling, and siloed coordination. Each new campaign, policy rollout, or service improvement required more people, more money, and more time.
But the future doesn’t have to look like the past. By layering Frontline-Aware AI™ into health engagement, we can move toward a new operating model:
- From linear processes to exponential workflows. Where once campaign planning and delivery dragged in a straight line, AI allows real-time orchestration across touchpoints, turning decision-making into a live, adaptive flow.
- From resource-intensive scaling to systems that grow without proportional cost. Instead of each new campaign demanding fresh budgets and full teams, AI-driven orchestration reuses data, automates validation, and delivers context-specific messaging at scale.
- From bottlenecks and delays to decentralization and agility. By shifting coordination closer to the frontline and empowering CHVs, clinicians, and caregivers with decision-support in their hands, systems become responsive to context, culture, and urgency.
This is more than an upgrade. It’s a transformation in how health systems think, act, and engage. The 3 waves of AI adoption in health delivery show us the trajectory: faster and cheaper, then better quality, then truly individualized engagement. By embracing this shift, we ensure that every message, every referral, and every decision can be as adaptive as the needs of the people we serve.
